Julie Entwistle, MBA, BHSc (OT), BSc (Health / Gerontology)
Co-authored by Angie Kingma, OT at 
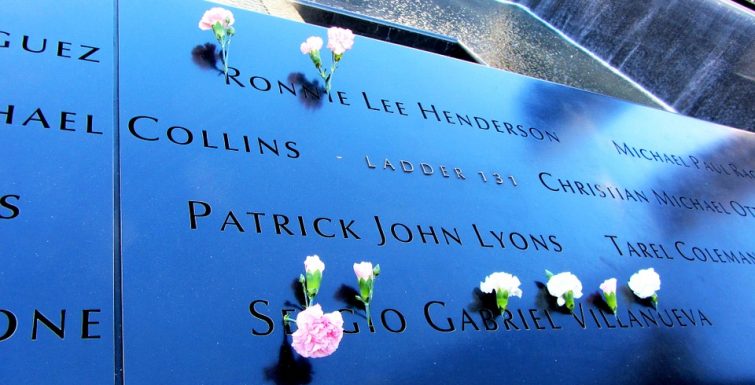
Every generation is said to be shaped, influenced and molded by the major world events that they experience. These events hit us so deeply that most of us can remember where we were when we “heard the news”, how we felt in the moment, and the way the world changed following the event. Today is the anniversary of 9/11 and marks a day of mourning for those of us that still feel deeply connected to the senseless tragedy that remains the world’s worst terrorist attack. But the threats aren’t over and the connected world we live in exposes all of us, including our children, to these events in gory detail complete with photos, video and even the live streaming of things as they unfold. If parents are not careful, these events can have a negative, harmful and life-lasting impact on children especially if we don’t help them process what they are seeing or hearing.
So, in the spirit of both mourning and hope, today I wanted to try and provide some suggestions on ways we can talk to our children about events like 9/11, the bombing at the Ariana Grande concert, North Korea testing missiles, the terrorism in Paris and London, attacks on Parliament Hill, or even the recent suffering caused by hurricane Harvey and the wildfires in Western Canada. Despite the fact that I am a mom of four, I still struggle to have these conversations with my kids, and as such reached out to an Occupational Therapist friend and colleague skilled in mindfulness (Angie Kingma www.mindfulnessforhealth.ca) to get her take on how all parents can try and manage these conversations better. Here is what Angie had to say:
Some parents take the stance that they’d rather shield their kids from the disturbing events that continue to happen daily around the world. These parents are well-meaning, assuming that talking about these grim facts will not only upset their kids but perhaps also cause harm. However, literature shows quite the opposite. What happens is that these kids are denied the opportunity to develop the resilience that is necessary to become a healthy, fully functioning adult. There are other parents who would like to discuss these issues but just don’t know what to say or where to start.
Mindful parenting can greatly enhance our ability to be skillful when talking to our kids about the world’s hard truths. So, what exactly is mindful parenting? It involves the intention to bring a particular quality of attention to the interactions with our children, as they unfold moment-by-moment. To do this, we choose to consciously pay attention to what is arising in the present moment, becoming aware of what’s happening internally for both the parent and the child, as well as what’s happening externally. Mindful attention is enveloped by attitudes of non-judgment, gentle curiosity, open-heartedness (kindness and compassion), as well as acceptance. We are especially interested in the child’s thoughts, feelings and bodily sensations, as well as our own. We practice mindful listening, which just means listening with full attention, staying present, conveying to your child that you are truly listening and care about their experience. This quality of focused attention and awareness goes beyond just listening to the words, and includes awareness of facial expressions and body language.
Here are some mindful communication tips when talking to kids about life’s difficulties:
Don’t avoid the conversation. Depending on your own comfort level, let kids know that darkness, misfortune, evil, natural catastrophes and other unpleasant life pressures do exist.
Explain issues to kids in an honest and age-appropriate manner.
Keep it simple. Kids don’t need the gruesome details, just the gist of the event. Find out what they know about it first and then fill in the gaps with the basics of what happened.
Remind your child that you might not have all the answers but that you know it’s important to have these types of discussions. Sometimes they aren’t looking for answers, our kids just need to feel “seen” and “heard”, and to feel a sense of safety.
Stay level-headed when you’re discussing difficult news. Practice ‘radical acceptance’ of these realities, which simply means acknowledging the truth of things (radical acceptance doesn’t mean we that we have to like it or approve).
Pay attention to your own feelings. Since events like terrorist attacks evoke strong emotions in us and our kids, be aware of what feelings are coming up in you before the conversation and during. Pay attention to your feeling(s) and observe them, breathing with them, without having to act on or get overwhelmed by them. When we can regulate our own feelings, it can help your child to regulate their own feelings (a term called “co-regulation”).
Share with your child what strategies you use to deal with distressing situations.
Seek professional assistance if you’re having feelings that are too difficult to manage on your own or your coping strategies are unhealthy or ineffective.
Pay attention to your child’s feelings. Help them name what they are feeling, which tips us in the direction of emotional regulation. Ask them if they can describe where in their body they feel their emotion, ex. tightening in chest, butterflies in the tummy, tension around their head.
Listen open-heartedly to your child’s feelings about the situation. Ask open-ended questions such as “How does hearing about this make you feel?” or “Is there anything else that you’d like to talk about?”
Validate your child’s feelings, even if you don’t understand them yourself. Say “Of course you’d feel that way. That makes total sense to me”.
If you notice a significant increase in fear and anxiety in your child that begins to affect their daily functioning, report this to your family doctor as soon as possible and consider getting a referral to a children’s mental health specialist.
Respect it if your child will simply not talk about certain topics. Some children, particularly kids who already have anxiety, won’t be able to tolerate the conversation so don’t force it. Other kids will have a lot to say and want to discuss it at length. Neither response is better than the other.
Difficulty helps to build our resilience. Let your child know that the things that we go through in life make us stronger and teach us important lessons. Point out specific stories of heroism, survivors, first responders or people coming together to help one another during times of need.
Teach the concept of impermanence, meaning that while difficulties in the world do exist in the present moment, things are always changing. There is hope that things will change for the better. Practice modelling attitudes of hope and optimism and discuss the importance of these with your child.
Not only does mindful parenting and communication strengthen the parent-child bond and facilitate a strong attachment, it also cultivates emotional awareness and self-regulation, which our world so desperately needs.
“Your mindful presence is the most valuable and precious gift you can give to yourself and to your children.”